Varicocele Diagnosis
What is a Varicocele?
A varicocele is caused by dilatation of the pampiniform plexus of spermatic veins (Figure 1). It is present in 15 to 20 % of post-pubertal males, 10-15% of unmarried military recruits, 35 % of infertile men who have never fathered a child and 81 % of men who were once fertile but are now infertile (secondary infertility). Left-sided varicoceles are 10 times more common than right-sided ones. They are commonly diagnosed clinically and on an ultrasound.
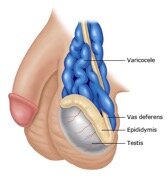
Figure 1. A varicocele is a collection of dilated and tortuous veins in the pampiniform plexus surrounding the spermatic cord. On physical examination, the spermatic cord has a “bag of worms” appearance that increases with standing or the valsalva manoeuvre.
The reason for the left-sided predominance may be explained anatomically. The left spermatic (gonadal) vein is one of the longest veins in the body, entering the left renal vein at a perpendicular angle. The intravascular pressure in the left renal vein is higher than on the right because it is compressed between the aorta and the superior mesenteric artery coming off the aorta above the renal vein, thereby producing a “nutcracker effect.” This phenomenon causes increased pressure in the left gonadal vein, which can dilate and cause incompetence of the valve leaflets, leading to retrograde flow of blood toward the testis in the erect position. The venous complex in the scrotum dilates and produces anything from minimal fullness on Valsalva manoeuvre to a large soft scrotal mass (“bag of worms”) that decompresses and disappears in the recumbent position.
Bilateral varicoceles occur in 33 %. Unilateral right varicoceles are very rare and may be associated with an underlying pathology causing inferior vena caval obstruction (renal cell carcinoma with IVC thrombus, right renal vein thrombosis with clot propagation down the IVC, etc).
Varicoceles are graded I, II, or III, according to size (Table 1).
| Grade | Size | Clinical description |
| 1 | Small | Palpable only with valsalva manoeuvre |
| 2 | Moderate | Nonvisible on inspection, but palpable upon standing |
| 3 | Large | Visible on gross inspection |
Table 1. Grading of varicocoeles
What are the symptoms?
Varicoceles may be asymptomatic (be without symptoms) or may cause any or all of the following:
- Dull, aching left scrotal pain, typically noticeable when standing and relieved by recumbency
- Feeling as though 1 testicle is heavier than the other
- Testicles that look different in size
- Testicular atrophy, believed to be secondary to loss of germ cell mass by induction of apoptosis (programmed cell death) initiated by the associated slightly increased scrotal temperature
- Compromised fertility
Although the presence of a varicocele can be associated with normal semen parameters and normal fertility, most men with varicocele and presumptive infertility have abnormal semen parameters, including low sperm concentration and abnormal sperm morphology. In a World Health Organization (WHO) study of over 9000 men who were partners in an infertile couple, a varicocele was much more common in men with abnormal semen (25.4 versus 11.7 % with normal semen). The causal relationship between varicocele and male infertility has been ascribed to increased testicular temperature, delayed removal of endogenously derived toxic materials and metabolites, hypoxia, and stasis (1).
Figure 1. A varicocele is a collection of dilated and tortuous veins in the pampiniform plexus surrounding the spermatic cord. On physical examination, the spermatic cord has a “bag of worms” appearance that increases with standing or the valsalva manoeuvre.
The reason for the left-sided predominance may be explained anatomically. The left spermatic (gonadal) vein is one of the longest veins in the body, entering the left renal vein at a perpendicular angle. The intravascular pressure in the left renal vein is higher than on the right because it is compressed between the aorta and the superior mesenteric artery coming off the aorta above the renal vein, thereby producing a “nutcracker effect.” This phenomenon causes increased pressure in the left gonadal vein, which can dilate and cause incompetence of the valve leaflets, leading to retrograde flow of blood toward the testis in the erect position. The venous complex in the scrotum dilates and produces anything from minimal fullness on Valsalva manoeuvre to a large soft scrotal mass (“bag of worms”) that decompresses and disappears in the recumbent position.
Bilateral varicoceles occur in 33 %. Unilateral right varicoceles are very rare and may be associated with an underlying pathology causing inferior vena caval obstruction (renal cell carcinoma with IVC thrombus, right renal vein thrombosis with clot propagation down the IVC, etc).
Varicoceles are graded I, II, or III, according to size (Table 1).
| Grade | Size | Clinical description |
| 1 | Small | Palpable only with valsalva manoeuvre |
| 2 | Moderate | Nonvisible on inspection, but palpable upon standing |
| 3 | Large | Visible on gross inspection |
Table 1. Grading of varicocoeles
What are the symptoms?
Varicoceles may be asymptomatic (be without symptoms) or may cause any or all of the following:
- Dull, aching left scrotal pain, typically noticeable when standing and relieved by recumbency
- Feeling as though 1 testicle is heavier than the other
- Testicles that look different in size
- Testicular atrophy, believed to be secondary to loss of germ cell mass by induction of apoptosis (programmed cell death) initiated by the associated slightly increased scrotal temperature
- Compromised fertility
Although the presence of a varicocele can be associated with normal semen parameters and normal fertility, most men with varicocele and presumptive infertility have abnormal semen parameters, including low sperm concentration and abnormal sperm morphology. In a World Health Organization (WHO) study of over 9000 men who were partners in an infertile couple, a varicocele was much more common in men with abnormal semen (25.4 versus 11.7 % with normal semen). The causal relationship between varicocele and male infertility has been ascribed to increased testicular temperature, delayed removal of endogenously derived toxic materials and metabolites, hypoxia, and stasis (1).
